CHILDHOOD DEPRESSION: COGNITIVE-BEHAVIORAL PLAY THERAPY

What is Childhood Depression?
Childhood depression is a psychological condition that affects a child’s emotions, behavior, and overall functioning.
In early childhood, emotion regulation is a dyadic process: the primary caregiver plays a fundamental role in helping children regulate and manage negative emotional states. Children show different predispositions to certain moods, but the central role of the parent in the relationship is to provide comfort for the child’s distress. Through repeated experiences of comfort, children learn that distress can be expressed to the caregiver and alleviated, and gradually over the first years of life children learn to manage frustration more independently, also thanks to the development of linguistic cognitive abilities.
The two major negative mood states, namely depression and irritability, are present in the experience of all individuals, including children. However, when depression and irritability are not merely transient emotional states but instead present as severe, poorly regulated, and prolonged, they may reflect the stabilization of a mood disorder.
When sadness and irritability are predominant in the child, especially if accompanied by symptoms such as insomnia, reduced appetite, and decreased activity level, a diagnosis of childhood depressive disorder should be considered.
How is Childhood Depression present?
Recognizing depression in children can be complicated because symptoms may vary from one child to another and may differ from those in adults. However, there are some common signs that clinicians and parents should know, including:
- Persistent sadness or depressed mood.
- Loss of interest in activities that previously brought pleasure.
- Changes in sleep or appetite patterns.
- Irritability and oppositional behavior.
- Low energy level and constant fatigue.
- Difficulty concentrating and poor school performance.
- Suicidal or self-destructive thoughts (more common in adolescents).
Children may lack the capacity to verbally express their emotional distress, so depressed mood can manifest as a persistently sad facial expression, tearfulness, and pervasive intensity across situations and relationships. Irritability may present as temper tantrums. Loss of pleasure in previously enjoyed activities is present and is associated with greater symptom severity, a family history of depression, and psychomotor delays.
These symptoms can appear in the child’s play and in marked changes in sleep, appetite, energy, and motor activity level.
When does Childhood Depression occur?
There is no specific age at which childhood depression universally manifests, but certain factors can increase the risk of developing depression at particular stages of a child’s life.
- Depression can occur already in the early years of life, even before school age. In this phase, symptoms may be harder to recognize due to young children’s limited ability to express emotions.
- Childhood depression may more commonly manifest during school age, when the child begins interacting with peers and faces social and academic challenges. The transition period between childhood and adolescence can be particularly difficult for some children.
- Adolescence is a period of major physical, emotional, and social changes, and many adolescents may experience depressive symptoms during this time. Increased academic pressures, relational challenges, and hormonal changes can contribute to the risk of depression in adolescence.
It is important to note that childhood depression can occur at any time following stressful events such as parental divorce, the loss of a loved one, moving to a new school, or bullying, and there is no single age at which it universally appears. Additionally, symptoms and severity can vary considerably from one child to another.
Being aware of early signs of depression and offering support and understanding to the struggling child can make a difference in their emotional well-being and healthy development. If parents suspect their child may be depressed, it is important to seek support from a mental health professional specialized in childhood and adolescent care for appropriate assessment and treatment.
What are the causes of Childhood Depression?
The causes of childhood depression are complex and may arise from a combination of genetic, biological, environmental, and psychological factors. It is important to emphasize that childhood depression can be multifactorial and that there is no single cause that explains all cases.
- Genetic factors: genetic predisposition can play a role in the onset of depression. Children with first-degree relatives who have a history of depression are at higher risk of developing the condition.
- Neurochemical dysfunctions: changes in brain neurotransmitters such as serotonin, norepinephrine, and dopamine can influence mood and contribute to the development of depression.
- Traumatic or stressful events: exposure to traumatic or stressful events—such as parental divorce, the loss of a loved one, moving to a new school, bullying, or abuse—can increase the risk of depression in children.
- Environmental factors: the family environment and the quality of relationships with parents and other family members can influence the child’s emotional well-being. For example, exposure to family conflict, emotional neglect, or an unstable family environment can increase the risk of depression.
- Biological factors: certain medical conditions or physical disorders, such as chronic illnesses, thyroid dysfunctions, or hormonal imbalances, can affect mood and increase the risk of depression in children.
- Insecure attachment styles: children who develop insecure attachment styles, such as anxious or avoidant attachment, may be more susceptible to depression.
- Psychological factors: low self-esteem, poor stress-coping abilities, persistent negative thoughts, or distorted thinking patterns can contribute to the development of depression in children.
Childhood Depression and Cognitive Behavioral Play Therapy (CBPT)
Cognitive Behavioral Play Therapy (CBPT) is an approach that aims to act on mood by first modifying behaviors and thought patterns, making the child an active participant in change. CBPT is a structured, brief, goal-oriented therapy whose objectives are shared with the child and the family. The child is welcomed into a play setting designed to create the therapeutic alliance, and parents follow a parallel pathway aimed at learning and strengthening parenting skills.
The intervention is organized into the following phases:
- ORIENTATION PHASE: This is the initial phase of CBPT. Significant emphasis is placed on preparing both the child and the parents. It is crucial to organize an initial meeting between the therapist and the parents, without the child present, to examine the child’s history and background information in detail. This allows parents to share their perception of the child’s problem. During these initial meetings, the therapist assists parents in preparing the child for the first session. In this phase, the ongoing role of parents and other significant adults in the assessment and treatment process is also explained. Although attention is focused on the child during CBPT, the therapist continues to interact regularly with the parents to offer support and to evaluate progress toward therapeutic goals.
- ASSESSMENT PHASE: This phase focuses on collecting crucial information to establish therapy goals. In addition to interviews with parents, a key element is observation of the child’s play. During this phase, various instruments are used, including questionnaires administered to parents, assessment of the child’s play, assessment of family play, the puppet sentence-completion task, and other measures personalized by the therapist. The therapist may establish a baseline for the frequency of the child’s behaviors, allowing evaluation of behavioral changes over the course of treatment.
- CASE CONCEPTUALIZATION PHASE: CBPT begins with analysis of the data collected during the child’s assessment, with the aim of planning an effective treatment and providing a logical structure for the development and achievement of therapeutic goals. The therapist starts by explaining childhood depression, analyzing individual, relational, and environmental factors related to the parents’ concerns. The emotional side, thoughts, physical sensations, and coping strategies used by the child are examined. This phase also includes analysis of protective, risk, and maintaining factors that contribute to the child’s behavior.
- INTERVENTION PHASE: The intervention phase of CBPT focuses on using CBT techniques that help the child with childhood depression develop more adaptive responses to problems, situations, and stressors. The emphasis is on learning more adaptive thoughts and behaviors. Methods used include modeling, role-playing, bibliotherapy, generalization, and relapse prevention. Interventions are often traditional cognitive techniques adapted through play tools such as drawing and expressive arts, listening to stories with therapeutic protagonists (therapeutic storytelling), or interacting with puppets that face similar situations. Treatment includes interventions aimed at helping the child generalize behaviors learned during sessions to other contexts and working on relapse prevention. Although the primary focus is on the child, it is important to maintain regular meetings with parents to monitor progress, assess and intervene in parent–child interactions, and provide guidance on areas of concern.
- CONCLUSION PHASE: Both the child and the family are actively involved in the final phase of therapy. During this final period, the child addresses feelings related to the end of therapy while the therapist highlights the changes that have occurred and consolidates the learning process. Final sessions may be extended over time, moving from weekly to biweekly or monthly meetings. This helps the child perceive their ability to manage life without the therapist. The therapist positively reinforces the child’s progress between sessions and seeks to normalize the experience of separation. Follow-ups are scheduled after the conclusion of the intervention at 3 months, 6 months, 12 months, and 24 months to verify the effectiveness of the intervention.
What are the Therapeutic Goals in the treatment of Childhood Depression?
In CBPT, goal-setting is shared with the child and their family. In the context of childhood depression, the following objectives are generally pursued:
- Teach children, through play sessions, skills that will help them understand, think about, interpret, and respond effectively to events in their world, thereby escaping negative thought and behavior patterns that have led to their depression.
- Develop and strengthen coping skills. Because depression is often associated with low self-esteem and self-efficacy, it is important to ensure that the depressed child develops abilities that increase confidence, competence, and empowerment.
- Develop problem-solving skills.
- Provide psychoeducation to both parents and the child. It is essential that parents understand this distinction when they begin to comprehend the specific challenges their children face. Even more importantly, both parents and the child should start with the awareness that the child is not responsible for the disorder, that symptoms are separate from who the child is as a person, and that all stakeholders (e.g., parents, teachers, therapists) assume responsibility for addressing current struggles.
What can Parents do?
It is essential that parents of depressed children understand the factors contributing to the child’s symptoms, the environmental cues and events that trigger mood changes, and behavior management strategies that enhance self-esteem rather than shame the child.
- Parents should be taught the principles of the collaborative problem-solving approach (Greene, 2014). This approach allows both parent and child to express their desires and needs and models a problem-solving method that respects both points of view in reaching a solution.
- Parents must understand that depression results in low motivation to participate in activities and that lack of participation worsens depression because it reduces opportunities for new learning.
- Parents should engage their depressed child in affectionate and supportive ways that convey the message that they understand the symptoms are not the child’s fault, while at the same time providing a variety of fun, creative, social, and relaxing activities for the child.
- It is essential that parents understand that depressed children refuse to participate in activities, but this refusal is part of the child’s depressive symptoms, and punishing the child risks further shaming them for their symptoms.
- Parents should set the child up for success by starting with very small demands, catching the child succeeding, and using positive reinforcement strategies to increase the likelihood that the behavior will recur.
- Parents should also be taught how to model emotion regulation, coping, and problem-solving skills at home.
- Parents must be aware of additional types of interventions to consider when the child’s symptoms do not sufficiently improve through therapy alone.
ENHANCE YOUR CHILD PSYCOTHERAPY SKILLS
COGNITIVE BEHAVIORAL PLAY THERAPY TRAINING
INTERVENTO DI PARENT TRAINING NELLA DEPRESSIONE INFANTILE
PARENT TRAINING INTERVENTION IN CHILDHOOD DEPRESSION
What is CBPT Parent Training?
Parent Training is a competence-based intervention model that starts from the assumption that families are capable of managing and addressing the problem, that all families have strengths, and that they can learn.
Parent training embedded within Cognitive Behavioral Play Therapy emphasizes the importance of involving parents in the playroom setting, where they have the opportunity to observe and progressively implement interventions to shape adaptive behaviors in the presence of the therapist. It highlights parents’ adaptability and learning capacity and aims to modify relational styles and attitudes that negatively influence children’s behaviors.
What Parents can do through this approach?
Parents, in this way, have the opportunity to:
- Learn new skills
- Acquire and practice specific techniques
- Receive individualized, ongoing feedback from the therapist to help them become more aware
- Learn to interpret more accurately their children’s emotions, concerns, and communication as expressed through play
This intervention program follows an integrated and innovative approach founded on the following frameworks:
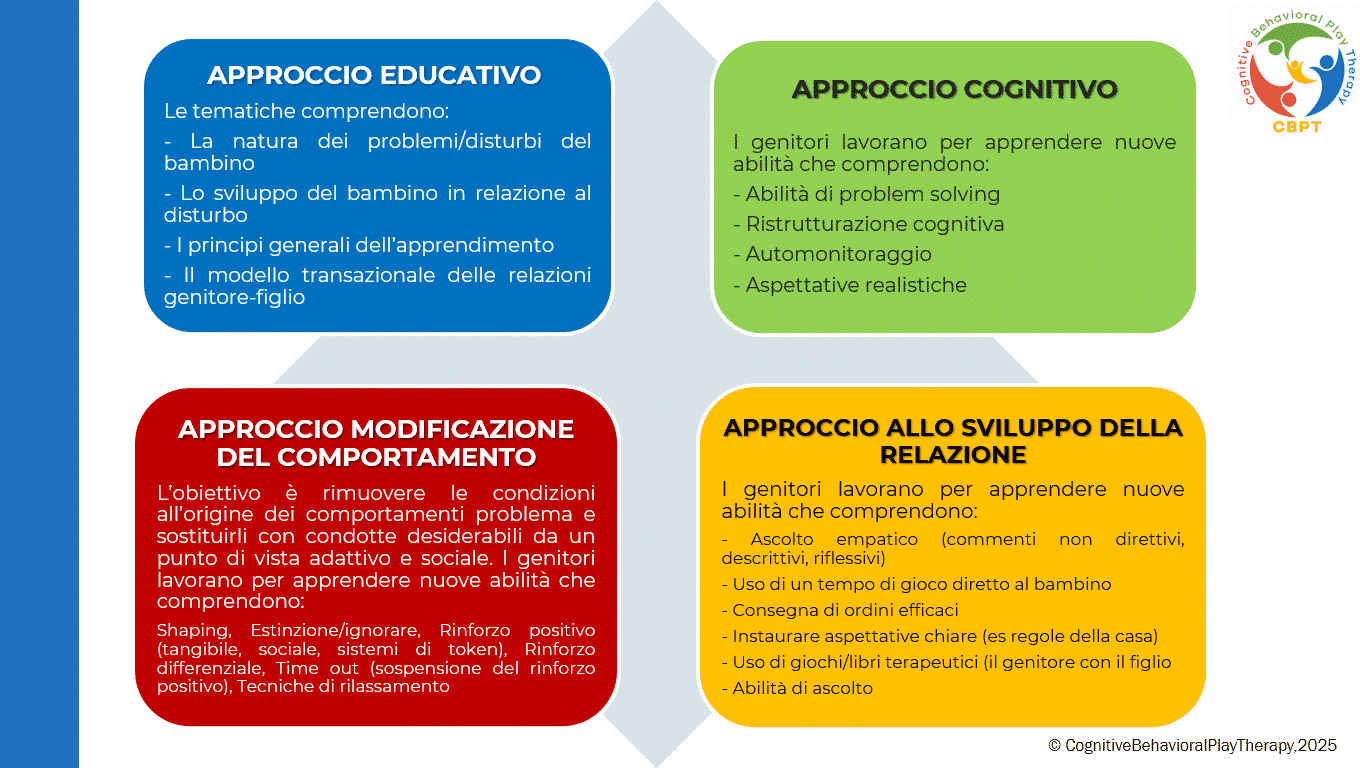
PARENT TRAINING IN COGNITIVE BEHAVIORAL PLAY THERAPY
Although the primary work is with the child, it is important to meet periodically with the parents. Parental involvement in cognitive-behavioral play therapy is important both during assessment and throughout treatment. A parallel pathway to the child’s therapy is planned, emphasizing the fundamental role of parents in influencing their children’s maladaptive behaviors. Parents are often encouraged to strengthen and reinforce the child’s adaptive behavior so that treatment continues outside the therapy setting (e.g., they are trained to use appropriate reinforcement for adaptive behaviors and extinction for maladaptive ones).
Target Population: Intended for both parents.
Duration: Typically 6 to 14 sessions, organized as one weekly session of 1 hour.
The program is organized into phases:
- ASSESSMENT PHASE: The problem is analyzed, parenting style is adapted, and therapeutic goals are defined. In this phase parents receive information about the causes and consequences of their children’s dysfunctional behaviors and learn to establish clear and consistent rules.
- LEARNING PHASE: This phase focuses on teaching new skills essential to support the child’s change. Parents have the opportunity to learn and practice techniques through practice sessions in which the therapist role-plays the child, guiding and instructing the parents. Specific targets include:
- Mastery of prerequisites
- Modeling of skills
- Role-playing
- Errorless learning
- Successive approximations (shaping)
- Feedback (verbal and social reinforcers; token economy)
- Practice
- PRACTICE PHASE: Parents conduct play sessions with their own children to put learned skills into practice. They learn to recognize and prevent situations that trigger difficult behaviors and to apply the same problem-solving strategies across different contexts. After initial practice moments with the therapist, parents begin to run play sessions individually with their children under the therapist’s supervision.
- FEEDBACK AND GENERALIZATION PHASE: Parents discuss with the therapist the play sessions carried out at home to learn how to generalize what they have learned. Strengths and any problems that arose are reviewed. The therapist helps parents generalize all learned interventions and the parenting skills acquired during training. Each week some time is dedicated to applying techniques in everyday life, and homework assignments are given to practice the strategies.
- CONCLUSION PHASE: This phase occurs when therapeutic goals have been met and parents have achieved a satisfactory level of competence regarding play activities and parenting skills. Therapy is often tapered gradually, reducing session frequency to alternate weeks, then monthly, and so on.
Objectives of Parent Training
This program helps parents interact effectively with their child by developing functional behavioral and communicative habits and techniques. The intervention aims to remove conditions that give rise to problem behaviors and to replace them with adaptive and socially desirable conduct. Objectives focus on preventing dysfunctions, promoting well-being, and improving crisis conditions.
Specific goals of work with parents include:
- Increase understanding of the child’s problematic behavior
- Establish more realistic expectations
- Enhance warmth, trust, and acceptance toward the child
- Recognize the importance of interaction through play
- Communicate more effectively with their children
- Develop greater parental confidence and reduce frustrations experienced with their children
- Cultivate greater patience to form more realistic expectations
- Discuss personal reactions with the therapist to develop deeper understanding of one’s own feelings and behaviors
- Learn to become effective problem solvers of family conflicts and increase motivation for change
Bibliography – References
American Psychiatric Association (2013) Diagnostic and Statistical Manual of Mental Disorders Fifth Edition DSM-5 Italian translation.
Berrini R. 2021 La collaborazione psichiatra/psicologo sulla gestione integrata dei casi in psicoterapia individuale Rivista semestrale di psicologia e psicoterapia individuale sistemica al tempo della complessità 7.
Favaro A., Sambataro F. 2021 Manuale di psichiatria. Piccin.
Geraci M. A. 2022 La play therapy cognitivo-comportamentale. Armando Editore.
Geraci M. A. 2023 Comprendere il mondo dei bambini giocando. Armando Editore.
Geraci M. A. 2024 Il mondo della dottoressa Lulù. Collana Amzon CBPT Books.
Greene, D. (1977). Social perception as problem solving. In J. S. Carroll & J. W. Payne (Eds.), Cognition and social behavior (pp. 277–283). Psychology Press.
Knell S. M. 1993 Cognitive Behavioral Play Therapy J. Aronson.